Acupuncture for Insomnia: How to Sleep Better Naturally
Sleep is fundamental to human health. It restores the body, regulates mood, and strengthens cognitive function. Yet millions of people struggle to get adequate rest. Insomnia, the persistent difficulty falling or staying asleep, has become one of the most common modern complaints. Studies suggest up to one in three adults experience insomnia symptoms at some point in their lives, with many turning to complementary health approaches for support (1).
Acupuncture, an ancient component of Traditional Chinese Medicine (TCM), has gained increasing attention for its potential to regulate sleep patterns through the body’s internal balance mechanisms. While more research is needed, evidence indicates acupuncture may influence neuroendocrine activity, stress responses, and the body’s natural circadian rhythms (2, 3).
This article provides an educational overview of insomnia, its relationship to TCM theory, and the growing body of scientific literature exploring acupuncture’s potential role in improving sleep quality.
Understanding Insomnia
Insomnia is more than just “a bad night’s sleep.” It refers to ongoing difficulty initiating or maintaining sleep that affects daytime function. The causes can be multifactorial: lifestyle factors (late-night screen use, caffeine, shift work), psychological factors (stress, anxiety), physiological imbalances (pain, hormonal fluctuations), or environmental triggers (noise, temperature).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines insomnia as difficulty sleeping for at least three nights per week, persisting for at least three months (4). Chronic insomnia can result in fatigue, concentration issues, and mood changes, and it has been associated with long-term impacts on immune, cardiovascular, and metabolic health (5).
The TCM Perspective on Sleep
Traditional Chinese Medicine interprets sleep through the lens of Yin-Yang balance and organ system harmony. Nighttime corresponds to Yin (rest), stillness, inward movement, while daytime is Yang (activity), alertness, outward expression. When Yin and Yang are unbalanced, or when vital substances such as Qi (energy) and Blood are deficient or obstructed, sleep disturbances may occur.
Common TCM patterns historically associated with insomnia:
心肝火旺 (Heart–Liver Fire Rising): agitation, irritability, restless dreams
心腎不交 (Heart–Kidney Disharmony): difficulty falling asleep, frequent waking, palpitations
氣血兩虧 (Qi–Blood Deficiency): light, dream-disturbed sleep, fatigue, pale complexion
痰熱擾心 (Phlegm-Heat Disturbing the Shen): heavy head, irritability, difficulty settling at night
In classical texts such as the Huangdi Neijing (Yellow Emperor’s Inner Canon), the concept of Shen (spirit or mind) is central. When Shen is settled, sleep comes naturally. When Shen is disturbed—by emotional strain, poor diet, or excess stimulation—the result is restlessness and insomnia.
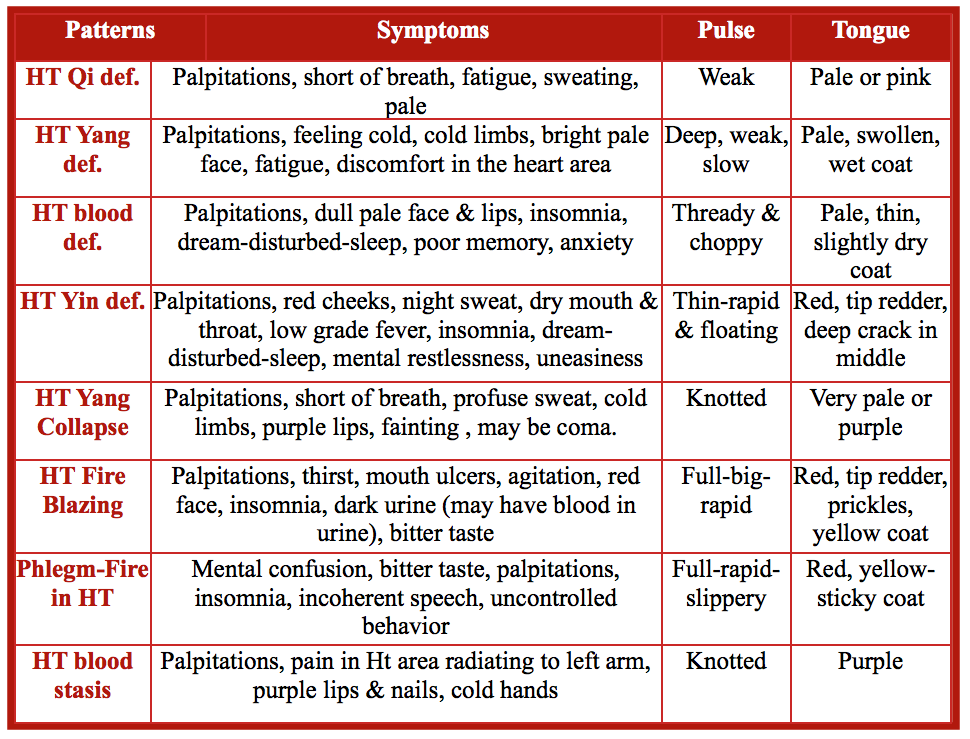
TCM Heart Patterns
Modern Research: How Acupuncture May Influence Sleep
Acupuncture involves stimulating specific points on the body to regulate physiological and energetic balance. Modern studies propose several mechanisms that may help explain its observed effects on sleep regulation:
Autonomic Nervous System Modulation:
Acupuncture has been observed to promote parasympathetic activation, supporting a shift from “fight-or-flight” toward “rest-and-digest” states (6). This modulation of autonomic tone may facilitate physiological relaxation before bedtime.Neurochemical Effects:
Research indicates acupuncture can influence neurotransmitters such as serotonin, dopamine, and GABA molecules intimately tied to mood and sleep cycles (7). Enhanced secretion of melatonin has also been reported in some clinical trials (8).Cortisol and Stress Hormones:
Chronic stress contributes to insomnia by elevating cortisol levels. Preliminary studies show acupuncture may help normalize cortisol rhythms, correlating with reduced anxiety and improved sleep quality (9).Brain Activity and Connectivity:
Functional MRI studies suggest acupuncture can modulate neural activity in brain regions related to emotion and circadian regulation, including the hypothalamus, amygdala, and hippocampus (10).Inflammatory and Pain Pathways:
Since pain and inflammation often interfere with sleep, acupuncture’s influence on endogenous opioid release and cytokine balance may indirectly support better rest (11).
Review of the Evidence
Scientific exploration of acupuncture and insomnia has accelerated over the last two decades.
A Cochrane systematic review analyzing randomized controlled trials found evidence suggesting acupuncture may improve subjective sleep quality scores compared with no treatment, though further high-quality studies are required (12).
A meta-analysis in Sleep Medicine reviewed data from over 3,800 participants and found significant improvements in Pittsburgh Sleep Quality Index (PSQI) and Insomnia Severity Index (ISI) outcomes across multiple studies (13).
Neuroendocrine research indicates acupuncture may increase nocturnal melatonin and reduce sympathetic activity, supporting biological plausibility (14).
Trials using electroencephalography (EEG) and polysomnography have observed increased deep sleep duration and reduced nighttime awakenings in some participants following acupuncture protocols (15).
While not every study shows uniform results, the cumulative literature suggests acupuncture may hold promise as a complementary approach to support sleep regulation. Researchers emphasize that larger, well-controlled studies are necessary to confirm efficacy and identify optimal parameters.
Integrating Good Sleep Practices
Beyond any therapeutic approach, long-term sleep quality depends on daily rhythms and lifestyle habits. Evidence-based strategies to promote better rest include:
Maintaining consistent bed and wake times—even on weekends.
Reducing screen time and bright light exposure before bed.
Avoiding heavy meals, alcohol, and caffeine late in the evening.
Creating a comfortable sleep environment (cool, dark, quiet).
Managing stress through mindfulness, breathing, or gentle exercise.
Traditional Chinese Medicine additionally highlights the importance of synchronizing with natural cycles—winding down after sunset, nourishing the body with warm foods, and balancing emotional expression during the day to quiet the mind at night.
Do’s and Don’ts for Insonmia
Future Directions in Research
Emerging investigations are examining how acupuncture may interact with:
Circadian gene expression—influencing molecular pathways like PER1 and CLOCK, which govern biological timing (16).
Gut–brain axis modulation, where acupuncture may affect microbiome activity and serotonin production relevant to sleep–mood interplay (17).
Combination therapies, such as integrating acupuncture with behavioral interventions (e.g., CBT-I) or mindfulness programs for synergistic outcomes (18).
Such research continues to expand understanding of how acupuncture fits into a comprehensive view of sleep health.
Conclusion
Acupuncture represents a complex, historically rooted system being studied through modern scientific frameworks. In the context of insomnia, research indicates possible effects on nervous system regulation, neurotransmitter balance, and sleep architecture.
While findings are encouraging, acupuncture for insomnia remains an area of active research rather than definitive treatment guidance. Individuals experiencing chronic sleep issues are encouraged to discuss options with qualified healthcare professionals and to maintain evidence-based sleep hygiene practices.
References
Ohayon MM. (2002). Sleep Medicine Reviews, 6(2), 97-111.
Zhao K. (2013). Acupuncture therapy for insomnia: a systematic review. Chinese Medicine, 8(1), 1-8.
Cao H et al. (2021). The role of acupuncture in treating sleep disorders: a review of clinical and neurobiological evidence. Frontiers in Neurology, 12, 680021.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.).
Vgontzas AN, Fernandez-Mendoza J. (2013). Sleep, 36(7), 1047-1055.
Huang W et al. (2011). Autonomic responses to acupuncture stimulation. Autonomic Neuroscience, 160(1-2), 1-10.
Zhan X et al. (2022). Effect of acupuncture on neurotransmitters in insomnia. Frontiers in Neurology, 13, 881420.
Spence DW et al. (2004). Acupuncture increases nocturnal melatonin secretion. J Neuropsychiatry Clin Neurosci., 16(1), 19-28.
Hsu CH et al. (2014). Acupuncture on cortisol levels in insomnia patients. Evid-Based Complement Altern Med., 2014, 243041.
Zhang R et al. (2023). Neural correlates of acupuncture for primary insomnia. Frontiers in Neuroscience, 17, 1113657.
Zhang X, Li P. (2018). Acupuncture and pain modulation: mechanisms of sleep improvement. Neural Plasticity, 2018, 7396418.
Cao H et al. (2009). Cochrane Database Syst Rev., (3), CD005472.
Dong B et al. (2022). Sleep Medicine, 90, 204-215.
Spence DW et al. (2004). J Neuropsychiatry Clin Neurosci., 16(1), 19-28.
Yeung WF et al. (2012). Sleep, 35(11), 1543-1551.
Li X et al. (2020). Acupuncture’s regulatory effects on circadian rhythm genes. Chronobiology International, 37(9-10), 1375-1388.
Chen J et al. (2021). Acupuncture and gut-brain axis: implications for sleep and emotion. Frontiers in Psychiatry, 12, 645594.
Wang Y et al. (2023). Integrative approaches combining acupuncture with CBT-I for insomnia. Complementary Therapies in Medicine, 75, 102938.